About My Work
I work in the ICU at Guthrie Robert Packer Hospital. I see a wide range of patients with medical, surgical and trauma issues. So this could be anyone from a cancer patient who is underweight, to a patient who had part of their small intestine removed, to a trauma patient who got in a car accident. I complete nutrition consults and nutrition screens within 72 hours of the patient's admission. Basically, this means I will visit any patient that the physician may notify us about who is eating poorly, needs alternative nutrition support, has lost weight or may be at risk for malnutrition. I determine patient's calorie, protein and fluid needs.
Nutritional Needs Assessment
There are many factors that affect the assessment of a patient's nutritional status. I do this by reviewing the patient's medical chart and assessing their previous medical history, disease state and severity, nutrition-related lab values, skin integrity and how much they are eating. For patients who can eat by mouth and are on a diet, I will visit and ask how they are eating and if they have any changes in their weight. To make sure these patients are adequately nourished, I may provide nutrition supplements like Ensure or Boost if they are not eating well. However, since I work in the ICU, the majority of my days are much more complex than this.
Challenges of Working in the ICU
A large handful of my patients are critically ill and are intubated. Patients who are intubated cannot eat by mouth, so my role as a Registered Dietitian is to provide something called "alternative nutrition support." This can be provided in two ways: from tube feedings or from TPN (which is essentially IV nutrition). There are many different types of tube feeding formulas. As an ICU dietitian, I determine which formula is best for my patient and how much to provide (in milliliters per hour). This can get tricky at times because I also need to assess if they are getting a sedative called Propofol, which actually provides fat calories. Then I have to take this in consideration when determining how much tube feeding or IV nutrition to provide to prevent overfeeding the patient. I make sure the tube feeding and IV nutrition meets the patient's protein and calorie needs. I also will have to review the patient's nutrition-related lab values, like sodium, potassium, etc., since it can be harmful if these are too low and high. Challenges I face in the ICU are patients who are not tolerating the tube feeding, and adjustments and interventions have to be made to correct this.
Best experiences in the program
I had a great in-person experience with the dietetic internship that is part of the three-semester program. I completed my clinical rotation at Bassett Medical Center in Cooperstown, NY. The staff there was very friendly, supportive and always had a positive attitude. I was able to apply the nutrition knowledge I learned from the graduate program to the hospital setting. I'm glad that I had the opportunity to visit patients and speak with them regarding their nutritional needs. It was validating knowing I could visit patients and provide quality nutrition care.
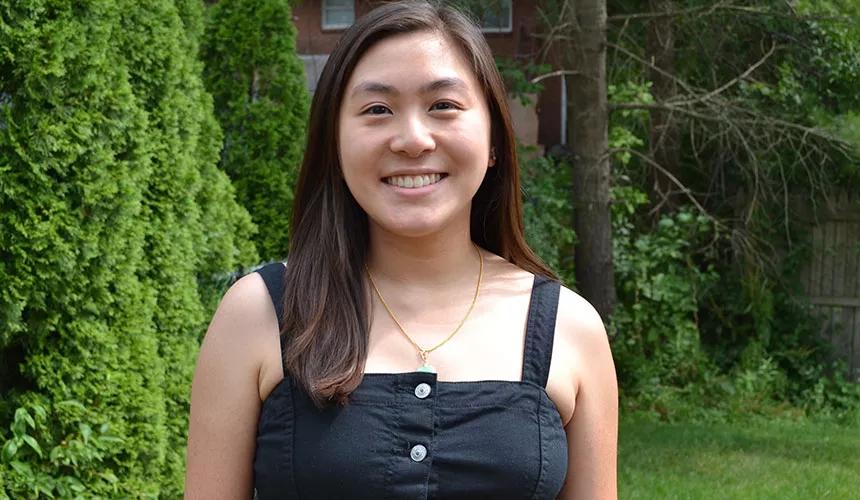
Why did you choose SUNY Oneonta?
I chose SUNY Oneonta's graduate program because I liked the appeal of an online program with a combined internship. It was very important to me to earn both a master's degree and complete my dietetic internship in order to become a Registered Dietitian. Another major factor of why I chose SUNY Oneonta's graduate program is because I knew almost all of the faculty from my undergraduate program in dietetics at SUNY Oneonta. I had excellent experiences with my professors throughout my undergraduate program. I enjoyed their courses, instruction style and how approachable they were. The nutrition and dietetics faculty members are not only sound instructors, but they provide an encouraging and supportive environment for their students. I knew by enrolling in this program, I would receive the high-quality education and support I would need to reach my career goals.
What’s the most rewarding aspect of your job?
The most rewarding part of my job is knowing that I am providing direct patient care to sustain a person's life. People often don't realize how important nutrition is. Since I work in the ICU, I am providing the necessary calories and protein for intubated patients who are not conscious to make decisions themselves. It's rewarding knowing that I am recommending and providing their source of energy and fuel. It would be different for a patient who CAN eat by mouth and is on a regular diet. I may recommend for the patient to consume 2,000 calories, but if the patient just isn't hungry and not feeling well, then there is no guarantee that they will actually meet their calorie needs. However, for critically ill intubated patients, I know that I am providing all their calorie and protein needs from the tube feeding and/or IV nutrition. Also, when COVID-19 was at its peak, Guthrie had a second ICU designated for just COVID patients. It was rewarding to know that I provided direct nutrition care for these patients.